Medically reviewed by Dr. Ramesh Gaddam, M.D. — Written by Sumalatha, D.N.H.E
Table of Contents
ToggleMilk intolerance, also known as lactose intolerance, is a condition where the body is unable to fully digest lactose, a sugar found in milk and dairy products. This occurs due to a deficiency of lactase, the enzyme responsible for breaking down lactose into simpler sugars that can be absorbed by the small intestine.
Symptoms of Milk Intolerance
The symptoms of milk intolerance, also known as lactose intolerance, typically occur within a few hours after consuming milk or dairy products.

Common symptoms include:
- Bloating
- Gas
- Abdominal pain or cramps
- Diarrhea
- Nausea
- Vomiting
- Bloating
Bloating:
Feeling uncomfortably full and swollen in the abdomen.
Gas:
Excessive gas production, leading to flatulence or belching.
Abdominal pain or cramps:
Sharp or dull pain in the abdomen, often centered around the lower abdomen.
Diarrhea:
Loose or watery stools may occur shortly after consuming dairy.
Nausea:
Feeling queasy or experiencing an upset stomach after consuming milk products.
Vomiting:
Some individuals may experience vomiting, particularly if they consume a large amount of dairy.
Lactose intolerance can also lead to symptoms such as fatigue, headaches, or irritability in some individuals, although these are less common and may be indirectly related to digestive discomfort.
Note:
It’s important to note that the severity and combination of symptoms can vary from person to person, depending on factors such as the degree of lactase deficiency, the amount of lactose consumed, and individual differences in digestive sensitivity.
If you suspect you have milk intolerance, it’s advisable to consult with a healthcare professional for proper diagnosis and management.
Causes of Milk Intolerance
Milk intolerance, also known as lactose intolerance, is caused by a deficiency or insufficiency of lactase, the enzyme responsible for breaking down lactose, the sugar found in milk and dairy products.

There are a few primary causes of lactase deficiency:
- Primary lactase deficiency
- Secondary lactase deficiency
- Congenital lactase deficiency
- Developmental lactase deficiency
Primary lactase deficiency:
This is the most common cause of lactose intolerance and occurs when the body produces less lactase enzyme with age. Many people are born with the ability to digest lactose, but as they get older, their bodies produce less lactase.
This type of lactase deficiency is more common in adulthood and can vary in severity among individuals and ethnic groups.
Secondary lactase deficiency:
This occurs as a result of an injury or illness that damages the small intestine, where lactase is produced.
Conditions such as celiac disease, Crohn’s disease, or intestinal infections can lead to temporary lactase deficiency until the intestine heals.
Congenital lactase deficiency:
In rare cases, some individuals are born with a genetic mutation that prevents the body from producing any lactase enzyme.
This condition, known as congenital lactase deficiency, is typically diagnosed early in infancy.
Developmental lactase deficiency:
Premature infants may experience temporary lactose intolerance due to underdevelopment of the small intestine, which can affect lactase production.
As the baby’s digestive system matures, lactase production usually increases, and symptoms of lactose intolerance subside.
Regardless of the cause, lactose intolerance results in undigested lactose reaching the colon, where it ferments and produces symptoms such as bloating, gas, abdominal pain, and diarrhea.
Management typically involves avoiding or reducing lactose-containing foods and using lactase supplements to aid in digestion.
Risk Factors of Milk Intolerance
Several risk factors can increase the likelihood of developing lactose intolerance:

Age:
Lactose intolerance is more common in adulthood, as the body naturally produces less lactase enzyme with age. Symptoms may appear during adolescence or adulthood, but they can vary in severity.
Ethnicity:
Certain ethnic groups have a higher prevalence of lactose intolerance. For example, lactose intolerance is more common among people of Asian, African, Hispanic, and Native American descent compared to individuals of European descent.
Family history:
Lactose intolerance can run in families. If one or both parents have lactose intolerance, their children may be more likely to develop the condition.
Premature birth:
Premature infants may have underdeveloped digestive systems, which can lead to temporary lactose intolerance. As their digestive systems mature, lactose intolerance symptoms typically improve.
Medical conditions affecting the digestive system:
Certain medical conditions, such as celiac disease, Crohn’s disease, or intestinal infections, can damage the lining of the small intestine and reduce lactase production, leading to lactose intolerance.
Gastrointestinal surgery:
Surgeries involving the stomach or intestines, such as gastric bypass surgery or intestinal resection, can affect lactase production and increase the risk of lactose intolerance.
Medications:
Some medications, such as antibiotics, can disrupt the balance of bacteria in the intestines, potentially leading to temporary lactose intolerance.
Radiation therapy:
Radiation therapy to the abdomen or pelvis can damage the lining of the intestines and reduce lactase production, resulting in lactose intolerance.
Understanding these risk factors can help individuals and healthcare professionals identify those who may be more susceptible to lactose intolerance and implement appropriate management strategies.
Complications of Milk Intolerance
Lactose intolerance itself is not typically considered a serious condition, but it can lead to certain complications if left unmanaged or if symptoms are severe. Some potential complications of lactose intolerance include:
Nutritional deficiencies:
Dairy products are significant sources of calcium, vitamin D, and other nutrients. If individuals with lactose intolerance avoid dairy products without replacing them with alternative sources of these nutrients, they may be at risk of deficiencies, particularly in calcium and vitamin D, which are essential for bone health.
Osteoporosis:
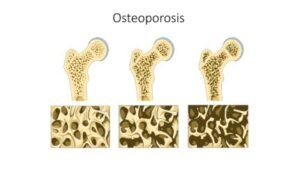
Chronic calcium deficiency due to inadequate intake of dairy products can increase the risk of developing osteoporosis, a condition characterized by weakened bones and an increased susceptibility to fractures.
Malnutrition:
Severe or prolonged lactose intolerance symptoms, such as diarrhea or vomiting, can lead to malabsorption of nutrients and subsequent malnutrition if not addressed promptly. This is more common in infants and young children with lactose intolerance.
Discomfort and reduced quality of life:
Untreated lactose intolerance can cause significant discomfort, including bloating, abdominal pain, gas, and diarrhea, which can interfere with daily activities and reduce quality of life.
Impact on social interactions:
Avoiding lactose-containing foods may limit social activities that involve dining out or attending events where dairy products are commonly served. This can lead to feelings of isolation or frustration.
Psychological effects:
Chronic symptoms of lactose intolerance may lead to feelings of frustration, embarrassment, or anxiety, particularly in social situations where dietary restrictions may be challenging to accommodate.
While lactose intolerance itself does not typically cause severe complications, it is essential to manage symptoms effectively through dietary adjustments, lactase enzyme supplements, or lactose-reduced dairy products to prevent potential complications and improve overall quality of life.
If individuals experience persistent or severe symptoms of lactose intolerance, they should consult with a healthcare professional for proper evaluation and management.
Diagnosis of Milk Intolerance
Diagnosing lactose intolerance typically involves a combination of medical history assessment, physical examination, and diagnostic tests. Here are the common approaches to diagnosing lactose intolerance:

Medical history assessment:
Healthcare providers will ask about symptoms, dietary habits, and any family history of lactose intolerance. They may inquire about the timing and severity of symptoms after consuming dairy products.
Physical examination:
A physical examination may be performed to assess for signs of lactose intolerance, such as abdominal bloating or discomfort.
Lactose intolerance elimination diet:
A healthcare provider may recommend temporarily eliminating lactose-containing foods from the diet to see if symptoms improve. If symptoms resolve during the elimination phase and reappear upon reintroducing lactose-containing foods, it suggests lactose intolerance.
Lactose tolerance test:
This test involves consuming a liquid containing lactose and then measuring blood glucose levels over several hours. If blood glucose levels do not rise significantly after consuming lactose, it indicates lactose intolerance.
Hydrogen breath test:
This test involves consuming a drink containing lactose, followed by measuring breath hydrogen levels over several hours. Elevated levels of hydrogen in the breath indicate undigested lactose in the colon, suggesting lactose intolerance.
Stool acidity test:
This test may be performed in infants and young children. It involves measuring acidity levels in stool samples after consuming lactose-containing formula or milk.
Genetic testing:
In some cases, genetic testing may be used to identify gene mutations associated with lactose intolerance, particularly congenital lactase deficiency.
It’s essential to consult with a healthcare professional for proper evaluation and diagnosis of lactose intolerance.
Other conditions, such as milk allergy or other gastrointestinal disorders, can have similar symptoms but require different management approaches.
Effective diagnosis allows for appropriate management strategies to alleviate symptoms and improve quality of life.
Treatment of Milk Intolerance
The primary treatment for lactose intolerance involves managing symptoms through dietary adjustments and, in some cases, using lactase enzyme supplements. Here are some common approaches to managing lactose intolerance:

Dietary modifications:
Limit or avoid foods and beverages that contain lactose, such as milk, cheese, yogurt, ice cream, and some processed foods.
Choose lactose-free or lactose-reduced dairy products, which have had the lactose partially or fully removed.
Substitute dairy products with lactose-free alternatives, such as plant-based milks (e.g., almond milk, soy milk) or lactose-free dairy products.
Gradually reintroduce small amounts of lactose-containing foods to gauge tolerance levels and identify individual thresholds.
Consume lactose-containing foods with other foods or meals to slow down digestion and reduce symptoms.
Lactase enzyme supplements:
Take over-the-counter lactase enzyme supplements before consuming lactose-containing foods or beverages to help digest lactose more effectively.
Follow the dosage instructions provided by the manufacturer or healthcare provider.
Probiotics:

Some research suggests that certain probiotic strains may help improve lactose digestion and reduce symptoms of lactose intolerance. Talk to a healthcare provider before trying probiotic supplements.
Be mindful of hidden sources of lactose:
Read food labels carefully to identify hidden sources of lactose in processed foods, medications, and supplements.
Ingredients such as whey, casein, and milk solids may indicate the presence of lactose in food products.
Manage symptoms:
Use over-the-counter medications, such as anti-gas products or anti-diarrheal medications, to alleviate symptoms if needed.
Stay hydrated and consume plenty of fluids to prevent dehydration, especially during episodes of diarrhea.
It’s essential to work with a healthcare provider or registered dietitian to develop an individualized management plan for lactose intolerance.
They can provide guidance on dietary modifications, recommend suitable lactase enzyme supplements, and monitor symptoms to ensure effective symptom management and nutritional adequacy.
In some cases, further evaluation or testing may be necessary to rule out other gastrointestinal conditions with similar symptoms.
Prevention of Milk Intolerance
Lactose intolerance is typically not preventable, as it is primarily due to genetics or age-related decline in lactase enzyme production. However, there are some strategies that may help manage symptoms and reduce discomfort associated with lactose intolerance:
Gradual introduction of dairy products:
Some individuals with lactose intolerance may be able to tolerate small amounts of lactose-containing foods without experiencing symptoms.
Gradually introducing dairy products into the diet and monitoring symptoms can help identify individual tolerance levels.
Choose lactose-free alternatives:
Opt for lactose-free or lactose-reduced dairy products, which have had the lactose partially or fully removed. These products are widely available and can be used as substitutes for traditional dairy items.
Use lactase enzyme supplements:
Taking over-the-counter lactase enzyme supplements before consuming lactose-containing foods or beverages can help improve lactose digestion and reduce symptoms of lactose intolerance.
Consume dairy with other foods:
Consuming lactose-containing foods with other foods or meals may help slow down digestion and reduce the likelihood of experiencing symptoms.
Pairing dairy products with foods that contain protein or fat can help buffer the effects of lactose.
Experiment with dairy alternatives:
Explore non-dairy alternatives, such as plant-based milks (e.g., almond milk, soy milk, coconut milk) or lactose-free dairy products, as substitutes for traditional dairy items.
These alternatives can provide similar nutritional benefits without the lactose.
Read food labels carefully:
Be mindful of hidden sources of lactose in processed foods, medications, and supplements. Ingredients such as whey, casein, and milk solids may indicate the presence of lactose in food products.
Monitor symptoms:
Keep track of symptoms after consuming dairy products or lactose-containing foods. This can help identify triggers and determine individual tolerance levels, allowing for better symptom management.
While lactose intolerance cannot be prevented, these strategies can help individuals manage symptoms and enjoy a varied and nutritious diet without discomfort.
It’s essential to work with a healthcare provider or registered dietitian to develop an individualized management plan tailored to specific needs and preferences.
Foods to Avoid
For individuals with lactose intolerance, it’s important to be aware of foods that contain high levels of lactose to avoid triggering symptoms. Here are some common foods and beverages that may contain significant amounts of lactose:
Dairy milk:

Cow’s milk and other animal-based milks contain lactose and may cause symptoms in lactose intolerant individuals.
Cheese:

Many types of cheese, especially soft cheeses like ricotta, cottage cheese, and cream cheese, contain lactose. However, aged cheeses typically have lower lactose content and may be better tolerated.
Yogurt:

While yogurt contains live cultures that can help digest lactose, it still contains lactose and may trigger symptoms in some individuals, particularly those with severe lactose intolerance.
Ice cream:

Ice cream and other frozen dairy desserts often contain high levels of lactose and can lead to symptoms in lactose intolerant individuals.
Butter and cream:

While butter and cream are lower in lactose compared to other dairy products, they still contain some lactose and may cause symptoms in sensitive individuals if consumed in large quantities.
Milk chocolate:

Chocolate containing milk or milk solids may contain lactose and should be avoided or consumed in moderation by individuals with lactose intolerance.
Processed foods:
Many processed foods, such as bread, cereal, salad dressings, and sauces, may contain hidden sources of lactose in the form of whey, casein, or milk solids. Reading food labels carefully is essential to avoid these sources of lactose.
Baked goods:
Some baked goods, such as muffins, cakes, and cookies, may contain milk or dairy ingredients that contribute to lactose content.
Instant mashed potatoes and pancake mixes:
These convenience foods often contain milk solids or whey powder, which can contribute to lactose content.
Cream soups and creamy sauces:
Cream-based soups and sauces may contain milk or cream, which can increase lactose content and trigger symptoms in individuals with lactose intolerance.
Note:
It’s important to note that lactose intolerance varies among individuals, and some people may tolerate small amounts of lactose-containing foods without experiencing symptoms.
Experimenting with portion sizes and observing individual tolerance levels can help identify which foods can be consumed comfortably.
Additionally, opting for lactose-free alternatives or using lactase enzyme supplements can help mitigate symptoms while still enjoying a varied and nutritious diet.
Non-Dairy Alternatives
For individuals with lactose intolerance or those who choose to avoid dairy products for other reasons, there is a wide range of non-dairy alternatives available that provide similar nutritional benefits. Here are some popular non-dairy alternatives to consider:
Plant-based milks:
Almond milk: Made from ground almonds and water, almond milk is low in calories and often fortified with calcium and vitamin D.
Soy milk: Made from soybeans and water, soy milk is a good source of protein and is often fortified with calcium and vitamin D.
Coconut milk: Made from the grated meat of coconuts and water, coconut milk has a rich flavor and creamy texture.
Oat milk: Made from oats and water, oat milk is naturally sweet and has a creamy texture. It’s often fortified with calcium and vitamin D.
Rice milk: Made from milled rice and water, rice milk has a mild flavor but is lower in protein compared to other plant-based milks. It’s often fortified with calcium and vitamin D.
Non-dairy yogurt:
Soy yogurt: Made from soy milk, soy yogurt is a creamy alternative to dairy yogurt and is available in various flavors.
Coconut yogurt: Made from coconut milk, coconut yogurt has a rich, creamy texture and a slightly sweet flavor.
Almond yogurt: Made from almond milk, almond yogurt is a nutritious alternative to dairy yogurt and is often fortified with probiotics.
Non-dairy cheese:
Soy cheese: Made from soy milk, soy cheese comes in various flavors and textures, including slices, shreds, and blocks.
Nut-based cheese: Made from nuts such as cashews, almonds, or macadamias, nut-based cheese is rich and flavorful, with a creamy texture.
Non-dairy ice cream:
Coconut milk ice cream: Made from coconut milk, coconut milk ice cream is rich and creamy, with a tropical flavor.
Almond milk ice cream: Made from almond milk, almond milk ice cream is lower in calories and fat compared to traditional dairy ice cream.
Soy milk ice cream: Made from soy milk, soy milk ice cream is a creamy alternative to dairy ice cream and is available in various flavors.
Non-dairy butter:
Plant-based butter: Made from oils such as coconut oil, soybean oil, or olive oil, plant-based butter is a versatile alternative to dairy butter and is suitable for cooking and baking.
These non-dairy alternatives are readily available in most grocery stores and provide options for individuals with lactose intolerance or those following a dairy-free diet.
When choosing non-dairy alternatives, it’s essential to look for products that are fortified with calcium, vitamin D, and other nutrients to ensure adequate nutrition.
Additionally, experimenting with different brands and flavors can help find alternatives that suit individual tastes and preferences.
Dairy Alternatives
Dairy alternatives are widely available and can provide similar taste and nutritional benefits as traditional dairy products. Here are some common dairy alternatives:
Plant-based milks:
Almond milk: Made from almonds and water, almond milk is low in calories and provides a nutty flavor. It is often fortified with calcium, vitamin D, and other nutrients.
Soy milk: Made from soybeans and water, soy milk is a good source of protein and is often fortified with calcium and vitamin D. It has a creamy texture and is suitable for various uses.
Coconut milk: Made from the flesh of coconuts and water, coconut milk has a rich, creamy texture and a slightly sweet flavor. It is commonly used in cooking and baking.
Oat milk: Made from oats and water, oat milk has a creamy texture and a mild, slightly sweet flavor. It is often fortified with calcium and vitamin D.
Plant-based yogurt:
Coconut yogurt: Made from coconut milk, coconut yogurt has a creamy texture and a mild coconut flavor. It is suitable for those following a dairy-free or vegan diet.
Soy yogurt: Made from soy milk, soy yogurt is a good source of protein and has a creamy texture similar to dairy yogurt. It is available in various flavors.
Plant-based cheese:
Nutritional yeast: Nutritional yeast is a deactivated yeast that is often used as a cheese substitute due to its savory flavor. It can be sprinkled on dishes or used to make dairy-free sauces and spreads.
Plant-based cheese alternatives: Made from nuts, seeds, or soy, plant-based cheese alternatives come in various flavors and textures, including slices, shreds, and blocks.
Plant-based butter:
Margarine: Margarine is a vegetable-based spread made from oils such as soybean, palm, or sunflower oil. It is commonly used as a dairy-free alternative to butter in cooking and baking.
Plant-based ice cream:
Coconut milk ice cream: Made from coconut milk, coconut milk ice cream has a creamy texture and a rich coconut flavor. It is available in various flavors, including chocolate, vanilla, and fruit.
Almond milk ice cream: Made from almond milk, almond milk ice cream is lower in calories and fat compared to traditional dairy ice cream. It is available in various flavors and is suitable for those with nut allergies.
These dairy alternatives are readily available in most grocery stores and provide options for individuals who are lactose intolerant, vegan, or simply prefer to avoid dairy products.
When choosing dairy alternatives, it’s important to look for options that are fortified with calcium, vitamin D, and other nutrients to ensure adequate nutrition.
Additionally, experimenting with different brands and flavors can help find alternatives that suit individual tastes and preferences.
Conclusion
Milk intolerance, or lactose intolerance, occurs when the body can’t fully digest lactose, a sugar in milk. This leads to symptoms like bloating, gas, and diarrhea after consuming dairy products. Management involves avoiding lactose-containing foods or using supplements to aid digestion.
Medically reviewed by Dr. Ramesh Gaddam, M.D.

General Physician, Diabetologist, and Critical Care Specialist.
Related
Discover more from Health Build-Up
Subscribe to get the latest posts sent to your email.
