Medically reviewed by Dr. Ramesh Gaddam, M.D. — Written by Sumalatha, D.N.H.E
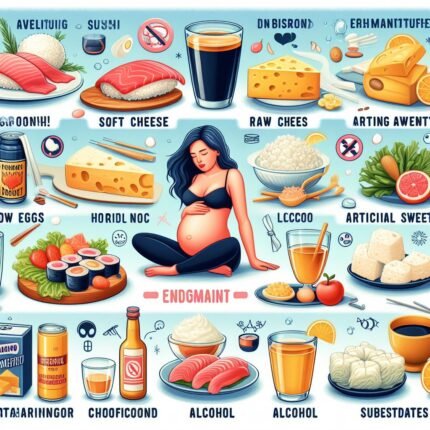
During pregnancy, dietary choices play a crucial role in maternal and fetal health. Certain foods pose potential risks and are best avoided to ensure a smooth pregnancy. Being mindful of what to exclude from your diet can contribute to a safer and healthier gestational experience. It’s important to be mindful of food choices to ensure the health and well-being of both the mother and the developing baby.
Foods to avoid during pregnancy
Following are the foods to avoid during pregnancy:
- High-Mercury Fish
- Raw or Undercooked Seafood and Eggs
- Unpasteurized Dairy Products
- Processed Meats and Deli Products
- High-Caffeine Beverages
- Raw Sprouts
- Excessive Vitamin A
- Alcohol
- Unwashed Produce
- Excessive Sugar and Junk Foods
1. High-Mercury Fish
High-mercury fish, including shark, swordfish, king mackerel, and tilefish, pose potential risks during pregnancy. These species contain elevated levels of mercury, a heavy metal known to adversely affect the developing baby’s nervous system.
Mercury’s Impact on Development:
1. Nervous System Concerns:
Mercury interference during pregnancy can negatively impact the formation of the baby’s brain and nervous system tissues. The developing fetus is particularly susceptible to the toxic effects of mercury, potentially leading to developmental issues and cognitive impairments.
2. Crossing the Placenta:
Mercury can easily cross the placenta, exposing the fetus to its harmful effects. Prolonged exposure increases the risk of adverse outcomes, emphasizing the importance of avoiding high-mercury fish to safeguard the baby’s neurological development.
Making Safer Seafood Choices:
1. Recommended Alternatives:
To mitigate mercury risks, opt for low-mercury fish alternatives such as salmon, trout, and shrimp. These options provide essential omega-3 fatty acids without the elevated mercury levels found in certain predatory fish.
2. Raw or Undercooked Seafood and Eggs
Steer clear of raw or undercooked fish, shellfish, and eggs to minimize the risk of foodborne illnesses such as salmonella during pregnancy.
Pregnancy demands a careful consideration of dietary choices to ensure the well-being of both mother and baby. One critical aspect involves avoiding raw or undercooked seafood, shellfish, and eggs to mitigate the potential risk of foodborne illnesses, particularly salmonella.
Risks of Raw or Undercooked Consumables:
1. Salmonella Concerns:
Raw or undercooked fish, shellfish, and eggs may harbor harmful bacteria, including salmonella. Ingesting these pathogens poses an increased risk of foodborne illnesses that can have adverse effects on the mother and the developing fetus.
2. Maternal and Fetal Health Impact:
Contracting foodborne illnesses during pregnancy can lead to dehydration, a compromised immune system, and, in severe cases, may even result in preterm birth or developmental complications for the baby. Hence, strict avoidance of undercooked consumables is vital.
Safe Practices for a Healthy Pregnancy:
1. Thorough Cooking:
Ensure that all seafood and eggs are thoroughly cooked to eliminate any potential pathogens. Cooking at recommended temperatures helps safeguard against harmful bacteria, reducing the risk of foodborne illnesses.
2. Mindful Food Handling:
Adopting proper food handling practices is essential. This includes storing perishables at appropriate temperatures, avoiding cross-contamination, and washing hands thoroughly before preparing or consuming meals.
3. Unpasteurized Dairy Products
Avoid unpasteurized milk, cheeses, and other dairy products to reduce the risk of infections like Listeria during pregnancy.
Pregnancy necessitates vigilant dietary choices, and one key consideration is the avoidance of unpasteurized dairy products. This precaution is essential to minimize the risk of infections, particularly Listeria, which can have serious implications for both the expectant mother and the developing fetus.
The Risks:
1. Listeria Threat:
Unpasteurized milk, cheeses, and other dairy products can harbor Listeria, a bacterium notorious for causing foodborne infections. Pregnant individuals are at an increased risk, as Listeria can lead to severe complications such as miscarriage, premature birth, or infections in newborns.
2. Maternal and Fetal Health Impact:
Contracting Listeria during pregnancy may result in flu-like symptoms for the mother, but the repercussions for the fetus can be severe. Listeriosis can lead to developmental issues, neurological problems, or even life-threatening conditions for the baby.
Practical Measures for a Safer Pregnancy:
1. Opting for Pasteurized Alternatives:
Choose pasteurized dairy products to ensure they have undergone a process that eliminates harmful bacteria. This significantly reduces the risk of infections, providing a safer option for both mother and baby.
2. Reading Labels:
Vigilantly read product labels to confirm the pasteurization status of dairy items. Clear labeling indicating pasteurization provides a reliable indicator of the product’s safety for consumption during pregnancy.
4. Processed Meats and Deli Products
Limit consumption of processed meats and deli products during pregnancy due to the potential risk of bacterial contamination.
Pregnancy prompts a careful evaluation of dietary habits, and one area of consideration is the consumption of processed meats and deli products. Limiting their intake is advised to mitigate potential risks associated with bacterial contamination, ensuring a healthier gestational period.
Identifying Potential Risks:
1. Bacterial Contamination Concerns:
Processed meats and deli products may pose a risk of bacterial contamination, particularly with pathogens like Listeria or Salmonella. Pregnant individuals are more susceptible to these infections, which can lead to serious complications for both mother and baby.
2. Maternal and Fetal Health Impact:
Bacterial infections from contaminated meats can result in foodborne illnesses with symptoms ranging from mild to severe. For pregnant women, these infections may increase the risk of preterm birth, miscarriage, or developmental issues in the fetus.
Practical Measures for Safe Consumption:
1. Moderate Intake:
Limit the consumption of processed meats and deli products to reduce exposure to potential contaminants. Opt for alternatives that are prepared and handled with strict hygiene standards.
2. Thorough Cooking:
If choosing processed meats, ensure they are thoroughly cooked to eliminate bacteria. Cooking at recommended temperatures helps safeguard against potential health risks associated with undercooked products.
5. High-Caffeine Beverages
Keep caffeine intake to about 200-300 milligrams per day, including coffee, tea, and certain energy drinks, to avoid potential complications during pregnancy.
As pregnancy brings about a spectrum of lifestyle adjustments, managing caffeine intake becomes a crucial consideration. It is advisable to limit daily caffeine consumption to around 200-300 milligrams, encompassing coffee, tea, and specific energy drinks, to minimize potential complications during this vital period.
Caffeine Risks:
1. Potential Complications:
Excessive caffeine intake during pregnancy has been linked to an increased risk of complications such as miscarriage and preterm birth. Monitoring and moderating caffeine consumption are key elements in ensuring a healthier gestational experience.
2. Impact on Fetal Development:
High levels of caffeine can cross the placenta, affecting the developing fetus. This may lead to slower fetal growth and, in rare cases, contribute to developmental issues. Maintaining a balanced caffeine intake is essential for both maternal and fetal well-being.
Practical Guidelines for Consumption:
1. Daily Limits:
Adhere to the recommended daily caffeine limits of 200-300 milligrams. This includes considering not just coffee but also other sources like tea and certain energy drinks. Being mindful of these limits helps minimize potential risks.
2. Reading Labels:
Check labels for the caffeine content of beverages and products. Understanding the caffeine content allows for informed choices, ensuring that the cumulative intake remains within the suggested range.
6. Raw Sprouts
Avoid raw sprouts like alfalfa and clover, as they may harbor harmful bacteria, posing a risk during pregnancy.
Pregnancy demands heightened attention to food safety, and one precautionary measure involves the avoidance of raw sprouts, including varieties like alfalfa and clover. These seemingly wholesome additions to salads and sandwiches can harbor harmful bacteria, presenting a potential risk during this critical period.
Bacterial Risks:
1. Bacterial Contamination Potential:
Raw sprouts have been associated with outbreaks of foodborne illnesses, primarily due to the favorable conditions for bacterial growth during their cultivation. The moist and warm environment provides an ideal breeding ground for pathogens like Salmonella and E. coli.
2. Maternal and Fetal Health Impact:
Consuming contaminated raw sprouts during pregnancy may lead to foodborne infections, with symptoms ranging from gastrointestinal distress to more severe complications. Expectant mothers are particularly vulnerable, as these infections can pose risks to both maternal and fetal health.
Practical Measures for Safety:
1. Opting for Cooked Sprouts:
Choose cooked sprouts over raw varieties to eliminate the risk of bacterial contamination. Cooking sprouts thoroughly ensures that any potential pathogens are neutralized, making them a safer option for consumption during pregnancy.
2. Mindful Ingredient Choices:
When dining out or preparing meals, be vigilant about the inclusion of raw sprouts. Requesting cooked alternatives or omitting raw sprouts from dishes helps reduce the risk of exposure to harmful bacteria.
7. Excessive Vitamin A
Avoid high doses of vitamin A supplements during pregnancy, as excessive amounts can be harmful to the developing fetus.
While vitamins are crucial for maternal and fetal health during pregnancy, caution is warranted, particularly with vitamin A supplementation. Avoiding high doses is essential, as excessive amounts of this vitamin can pose potential harm to the developing fetus.
Understanding the Risks:
1. Developmental Concerns:
High doses of vitamin A during pregnancy have been linked to developmental issues in the fetus. Excessive amounts can disrupt the delicate balance required for proper fetal growth, potentially leading to birth defects.
2. Impact on Organ Systems:
Vitamin A is essential for the development of various organ systems in the fetus. However, an excess can tip the balance, potentially leading to malformations and complications in organs such as the heart, lungs, and central nervous system.
Practical Guidelines for Supplementation:
1. Recommended Daily Allowance:
Adhere to the recommended daily allowance (RDA) for vitamin A during pregnancy. This includes considering both dietary sources and any supplements, ensuring that the total intake remains within safe limits.
2. Consultation with Healthcare Providers:
Seek advice from healthcare professionals before taking vitamin A supplements during pregnancy. Individual health conditions and dietary habits can influence recommendations, making professional guidance essential.
Balanced Nutritional Approach:
1. Dietary Sources of Vitamin A:
Focus on obtaining vitamin A through a balanced diet rich in fruits, vegetables, and dairy products. This ensures a natural and regulated intake, reducing the need for additional supplements.
2. Varied Nutrient Intake:
Maintain a well-rounded diet that includes a variety of essential nutrients. A diverse range of foods contributes to overall maternal and fetal well-being without the potential risks associated with excessive vitamin A supplementation.
8. Alcohol
Completely abstain from alcohol during pregnancy to prevent birth defects and developmental issues.
choices regarding lifestyle habits, including alcohol consumption, play a pivotal role in ensuring the well-being of the developing fetus. The unequivocal recommendation is to completely abstain from alcohol to prevent the risk of birth defects and developmental issues.
Understanding the Risks:
1. Birth Defects and Cognitive Impairment:
Alcohol is known to cross the placenta, impacting fetal development. Exposure to alcohol during pregnancy increases the risk of birth defects, cognitive impairment, and developmental issues in the baby.
2. Fetal Alcohol Spectrum Disorders (FASD):
Consistent alcohol consumption during pregnancy can lead to Fetal Alcohol Spectrum Disorders (FASD), a range of conditions that may manifest as physical, behavioral, and intellectual challenges for the child.
Practical Measures for a Safe Pregnancy:
1. Complete Abstention:
The safest approach is to abstain entirely from alcohol during pregnancy, regardless of the type or quantity. This minimizes any potential risks and ensures a healthier gestational experience.
2. Support Systems:
Communicate the decision to abstain from alcohol to healthcare providers, friends, and family. Building a supportive environment contributes to a stress-free pregnancy, enabling better adherence to this crucial recommendation.
Zero Compromise for a Healthy Start:
Abstaining from alcohol during pregnancy is a non-negotiable choice for ensuring the optimal health and development of the baby. By embracing complete abstention, seeking professional guidance, and fostering a supportive environment, expectant mothers contribute to a safer and healthier gestational journey.
9. Unwashed Produce
Thoroughly wash fruits and vegetables to reduce the risk of exposure to pesticides and harmful bacteria during pregnancy.
As expectant mothers navigate the dietary landscape during pregnancy, a crucial aspect is ensuring the safety of fruits and vegetables. Thoroughly washing produce is a simple yet effective measure to minimize the risk of exposure to pesticides and harmful bacteria, promoting a healthier gestational experience.
Understanding the Risks:
1. Pesticide Residue Concerns:
Fruits and vegetables may carry traces of pesticides used in cultivation. While these chemicals are intended to protect crops, residual amounts can pose potential risks when consumed, particularly during pregnancy.
2. Bacterial Contamination:
Produce can harbor harmful bacteria, such as E. coli or Salmonella, which may lead to foodborne illnesses. Pregnant individuals are more susceptible, making thorough washing an essential practice for reducing these risks.
Practical Measures for Safer Consumption:
1. Thorough Washing Techniques:
Adopt thorough washing techniques for fruits and vegetables. Running them under cold water and using a soft brush for items with a tougher exterior can help remove surface pesticides and bacteria effectively.
2. Peeling and Cutting:
Consider peeling or cutting outer layers of fruits and vegetables when applicable, as this can further reduce pesticide and bacteria exposure. Discarding outer leaves or skins can be an added precautionary step.
Maintaining a Safe Dietary Environment:
1. Storage Practices:
Implement proper storage practices to maintain the freshness and safety of produce. Refrigerate perishable items promptly and be mindful of the shelf life of different fruits and vegetables.
2. Farmer’s Markets and Organic Options:
Consider exploring farmer’s markets or opting for organic produce, which may have lower pesticide residues. Engaging with local and organic options supports both safety and sustainability.
10. Excessive Sugar and Junk Foods
Limit the intake of sugary and processed foods during pregnancy, opting for a well-balanced diet rich in nutrients.
As the nutritional needs of pregnancy demand careful attention, curbing the consumption of excessive sugar and processed foods emerges as a key dietary guideline. Prioritizing a well-balanced diet, abundant in nutrients, promotes a healthier gestational journey for both mother and baby.
Understanding the Risks:
1. Impact on Maternal Health:
Excessive sugar and junk food intake can contribute to weight gain, gestational diabetes, and other health issues for expectant mothers. Maintaining a healthy weight is crucial for a smoother pregnancy experience.
2. Fetal Development Concerns:
High levels of added sugars and processed foods have been linked to adverse effects on fetal development. This includes an increased risk of childhood obesity, which may manifest later in the child’s life.
Practical Measures for a Balanced Diet:
1. Nutrient-Rich Alternatives:
Opt for nutrient-rich foods that provide essential vitamins and minerals. Incorporate a variety of fruits, vegetables, whole grains, lean proteins, and dairy products to meet the increased nutritional requirements during pregnancy.
2. Moderation in Treats:
While occasional indulgence is acceptable, moderation is key. Limit the intake of sugary and processed treats, choosing healthier alternatives when cravings arise.
Creating a Nourishing Environment:
1. Meal Planning:
Plan well-balanced meals to ensure a consistent intake of nutrients throughout the day. Preparing meals at home allows for better control over ingredients and helps avoid the excesses found in many processed foods.
2. Hydration with Water:
Stay hydrated with water instead of sugary beverages. Adequate water intake supports overall health and helps prevent unnecessary calorie consumption from sweetened drinks.
Always consult with a healthcare professional or a nutritionist for personalized advice based on individual health conditions and needs during pregnancy.
Conclusion
Medically reviewed by Dr. Ramesh Gaddam, M.D.

General Physician, Diabetologist, and Critical Care Specialist.
Discover more from Health Build-Up
Subscribe to get the latest posts sent to your email.