Medically reviewed by Dr. Ramesh Gaddam, M.D. — Written by Sumalatha, D.N.H.E
7. Functions of Cholesterol in the Body
Cholesterol is important for several aspects of good health.
- Cell Building and Repair: Cholesterol helps form and repair cell membranes, keeping cells stable and flexible.
- Hormone Production: Cholesterol is needed to make hormones like estrogen and testosterone, which help control growth, metabolism, and stress.
- Bile Production: Cholesterol helps produce bile, a substance that aids in digesting fats and absorbing nutrients from food.
- Vitamin D Production: Cholesterol helps your body make vitamin D when your skin is exposed to sunlight. Vitamin D is important for strong bones and a healthy immune system.
- Organ Function: Cholesterol supports the health of various organs, including the liver and brain, helping them work properly.
Overall, cholesterol is essential for many body functions, but it’s important to keep it balanced for good health.
8. Effects of High Cholesterol
Cognitive Impairment
High cholesterol can affect brain health. High levels of LDL (bad cholesterol) may lead to memory problems and cognitive decline.
This is because excess cholesterol can cause plaque buildup in the brain, potentially increasing the risk of conditions like dementia and Alzheimer’s disease.
Keeping cholesterol levels under control is important for maintaining good brain function and reducing the risk of these cognitive issues.
Digestive System
High cholesterol can also impact your digestive health.
Too much cholesterol can lead to the formation of gallstones, which are hard deposits that can block bile ducts.
This blockage can cause pain, inflammation, and digestive troubles.
Since cholesterol is used to make bile, an imbalance can disrupt fat digestion and nutrient absorption.
Managing cholesterol helps prevent gallstones and supports a healthy digestive system.
9. Cholesterol Myths and Misconceptions
Cholesterol is often misunderstood, leading to several myths that can affect dietary choices and health decisions. Here are some common misconceptions:
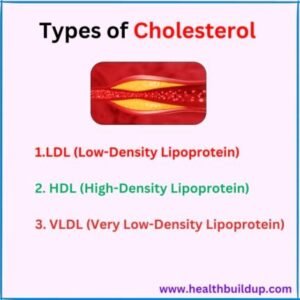
Myth 1: All cholesterol is bad.
Many people think that all cholesterol is harmful, but the body actually needs cholesterol for important functions, such as making hormones and maintaining cell membranes.
It’s crucial to distinguish between “good” (HDL) cholesterol and “bad” (LDL) cholesterol.
Myth 2: Eating cholesterol-rich foods raises blood cholesterol levels.
While the cholesterol you eat can affect your blood cholesterol, it’s not as significant as once believed.
For most people, saturated and trans fats in the diet have a bigger impact on raising LDL cholesterol.
Myth 3: High cholesterol only affects older adults.
High cholesterol can affect people of all ages, including children and young adults, especially if they have risk factors like obesity, poor diet, or a family history of high cholesterol.
Myth 4: You can’t lower cholesterol without medication.
Although medications can help, lifestyle changes such as improving your diet, exercising regularly, and managing your weight can also lower cholesterol levels effectively.
Many people achieve healthy cholesterol levels through these natural methods.
10. Impact of Age and Gender on Cholesterol
Cholesterol levels can vary based on age and gender, which can influence heart health risks:
Age:
As people get older, their cholesterol levels often rise due to changes in metabolism and hormones.
LDL cholesterol levels may increase, while HDL cholesterol levels might decrease, raising the risk of heart disease in older adults.
Gender:
Before menopause, women usually have lower total cholesterol levels compared to men.
After menopause, women’s LDL cholesterol levels often rise, and HDL levels may drop, increasing the risk of heart disease. Hormonal changes during menopause can affect how cholesterol is processed.
Monitoring:
Regular cholesterol checks are important for both men and women, especially as they age. Understanding how age and gender affect cholesterol can help people take proactive steps to manage their heart health.
11. Cultural and Ethnic Variations in Cholesterol Levels
Cholesterol levels can vary among different cultural and ethnic groups due to diet, lifestyle, and genetics:
Dietary Influences:
Different cultures have unique diets that can affect cholesterol levels.
For example, diets high in saturated fats and processed foods may lead to higher LDL cholesterol.
In contrast, diets rich in fruits, vegetables, whole grains, and healthy fats (like the Mediterranean diet) can promote better cholesterol profiles.
Genetic Factors:
Genetics play a role in how cholesterol is processed in the body. Some ethnic groups are more likely to have high cholesterol levels.
For example, people of South Asian descent often have higher LDL cholesterol and a greater risk of heart disease.
Health Disparities:
Recognizing these variations is important for developing health programs and educational efforts that address specific risks in different communities.
Culturally tailored dietary advice can help improve cholesterol management and overall heart health.
12. Recent Research and Studies on Cholesterol
Ongoing research continues to explore cholesterol and its effects on health:
Cholesterol and Heart Disease:
Recent studies confirm the link between high LDL cholesterol and an increased risk of heart disease.
Lowering LDL cholesterol through diet and medications has been shown to reduce the risk of cardiovascular problems.
Role of Inflammation:
New research highlights that inflammation may play a role in how cholesterol affects health.
Chronic inflammation can contribute to artery damage and heart disease, suggesting that managing inflammation is important for cholesterol control.
Dietary Fats:
Recent studies are examining how different types of dietary fats impact cholesterol levels.
Replacing saturated fats with unsaturated fats (found in foods like olive oil and nuts) has been shown to improve cholesterol levels.
Genetic Research:
Advances in genetics are helping identify people at higher risk for high cholesterol and heart disease.
Genetic testing can offer insights into how a person’s body processes cholesterol, allowing for more personalized and effective treatment plans.
These insights provide valuable information for managing cholesterol and making informed health decisions.
Conclusion
Medically reviewed by Dr. Ramesh Gaddam, M.D.

General Physician, Diabetologist, and Critical Care Specialist.
Discover more from Health Build-Up
Subscribe to get the latest posts sent to your email.


Pingback: ldl normal cholesterol levels : Importance and Management
Pingback: Grade 1 Fatty Liver: Causes, Symptoms, and Treatment
Pingback: HDL : How to increase HDL Cholesterol with Indian Food
Pingback: Cluster Beans (Guar) Nutrition Health Benefits, Side Effects
Pingback: Myocardial Infarction: Causes, Symptoms, and Treatment
Pingback: Gallbladder Stones: Symptoms, Causes, Types, Treatment, Diet
Pingback: Cardiovascular Diseases: Causes, Signs & (9 Prevention Tips)
Pingback: Childhood Obesity: Causes, Risks, Prevention (10 Best Tips)